Working to find your BEST WEIGHT is tough enough in itself. Unfortunately, certain ‘internal states’ can make this process even more difficult. Within this module you will be introduced to a finite list of modulators that can be obstacles between you and your BEST WEIGHT. Any weight management effort may be negatively affected by:
Not everyone who has overweight/obesity is negatively affected by every modulator, and therefore you should be supported in a personalized discovery and review of each one and how they apply to you.
Managing these barriers starts with understanding how they work. Fortunately, this is not complicated. You are reminded that overeating is driven by both the GATEKEEPER (hypothalamus/homeostatic system) and the GOGETTER (the motivation/reward system), and the only thing we have to stand up to it all is the Sleepy Executive (executive system).
The risk of the modulators is that they will do one of these three things.

Increase activity of the GATEKEEPER

Increase the learning and strength of the GOGETTER

Increase the sleepiness of the Sleepy Executive, leaving the executive system’s autopilot with free reign
All effective weight management strategies should regularly consider and revisit this list of modulators as possible obstacles and targets of intervention.
Stress is your body’s response to challenge or demand. In short bursts, stress can be positive, helping you overcome an acute threat or challenge. If prolonged, however, stress can affect quality of life, health and weight. Stress plays a role in the development of overweight and obesity across a number of pathways. Our stress system evolved to help us escape life-threatening situations; stress will dump glucose into our bloodstream so that muscles have energy for fight or flight. However, in the modern world, most stress is psychological, yet our bodies respond as if the challenge were a physical one.
-
Epidemiological studies show an association between stress and weight
-
Meta-analysis shows a relationship between stress and weight gain
Stress results in the release of the cortisol hormone from our adrenal glands and promotes fat gain within the abdominal cavity, depositing the unhealthy version of fat—the fat within the centre of the body.
Stress and the GOGETTER. The motivation system (the GOGETTER) is temporarily, directly and indirectly strengthened by stress.
Stress directly increases the neurotransmitter dopamine, which directly raises WANTING. Indirectly, stress results in the release of cortisol, which then directly makes the motivation system (the GOGETTER) more sensitive to cues in the environment that activate it, as well as strengthening WANTING.
The hormones leptin and ghrelin also react to stress. Leptin and ghrelin affect weight in opposite ways, with leptin suppressing appetite and ghrelin stimulating it. Ghrelin stimulates the GOGETTER and leptin sedates it.

Differences in leptin responses to stress may be associated with individual differences, which determine whether stress generates weight gain or weight loss. Stress raises leptin, and higher leptin responses to stress may protect against weight gain. Ghrelin levels also increase in stress conditions, which could promote weight gain.
Under stressful circumstances, high-calorie, hyper-palatable foods are preferred. If this is not unfair enough, this type of eating under the influence of stress can further program, strengthen and chronically sensitize the GOGETTER, thereby progressively and chronically strengthening WANTING.
Stress and the Sleepy Executive. Stress can significantly undermine restraint over WANTING. Early life stress can be particularly damaging to executive self-regulation skills. Stress directly decreases executive functioning and self-regulation, making the Sleepy Executive unmistakably sleepier.
Stress and weight bias. People living with overweight and obesity may frequently experience weight bias, stigma and discrimination. Weight bias relates to the negative weight-related attitudes, beliefs and assumptions about people with overweight and obesity. Evidence points to the stressful nature of the experience of weight bias as having a negative effect on all the above pathways, which can challenge weight loss and lead to further weight gain. The stress of weight bias has been demonstrated to create a vicious cycle where stress can lead to weight gain, which can lead to stress and so on.
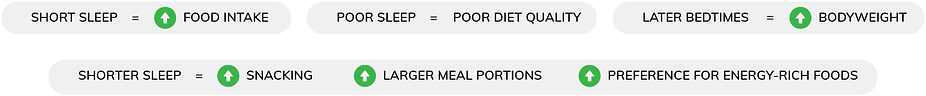
Disturbed sleep and fatigue. Decades of evidence now describe an association between sleep and eating.
As described by Jean-Philippe Chaput:
It may not be that easy to study, but the majority of the evidence suggests that short sleep duration is a causal force in weight gain and an obstacle to weight loss. Less sleep is simply considered a part of modern living. There is a growing consensus that short sleep duration is not only associated with weight but also with type 2 diabetes, heart disease, hypertension and mortality.
The association between weight and sleep can be understood by describing the effects of short sleep duration on the three levels/characters of the appetite system.
The GATEKEEPER
As a reminder, the GATEKEEPER defends against weight loss by responding to lower leptin levels. A landmark study by Karine Spiegel showed that two days of shorter sleep duration than the recommended number of hours induced an 18% drop in leptin. The same study also showed that short sleep duration increased the hunger/WANTING hormone, ghrelin, by 28%, and these hormone changes were also associated with reports of increased sensations of hunger and appetite.
The GOGETTER
Functional MRI is a form of MRI that is used in real time to show changes in brain activity in response to stimuli. Functional MRI studies are providing evidence that short sleep duration enhances the activity of the GOGETTER.
You will be reminded that the GOGETTER is the underlying drive to consume calories, also known as WANTING, and the GOGETTER represents the motivation or reward system—the middle layer of the three-layer human appetite system.
Short sleep duration in these studies is associated with
-
greater activation of the motivation system
-
a greater sensitivity to images of calorie dense and tasty foods that goes away with normal sleep
Taken together, this suggests that a short sleep duration can result in more persistent and taller waves of WANTING sent up to the executive system.
The Sleepy Executive
Studies also suggest that sleep restriction alters the sleepiness of the Sleepy Executive. Remember, the Sleepy Executive is the restraint and inhibition region of our executive system that challenges the automatic permission thoughts from our autopilot.
FMRI studies confirm that sleep deprivation reduces activity in areas that are associated with restraint and inhibition. Studies show that sleep-restricted adolescents eat foods higher in quick energy, and that sleep-restricted adults show less activity in the areas of inhibition and food intake increases. This all suggests that short sleep duration significantly makes the already Sleepy Executive sleepier.
Also of note, it is suggested that short sleep duration increases dangerous intra-abdominal fat and is associated with hyperactivity of the “stress circuit” called the HPA-axis, resulting in increased release of the stress hormone cortisol.
The relationship between depression and weight can be thought of as bi-directional, meaning that having one increases your risk of the other. A 2010 systematic review and meta-analysis that studied over 58,000 people suggested that obesity increases the risk of depression, and depression was predictive of developing obesity.
You may be surprised to learn that with depression, not everyone is at risk of weight gain. Some people with depression increase appetite and weight, and others actually find the opposite—decreased appetite and weight loss.
You may not be surprised to know that according to FMRI evidence, the GOGETTER is responsible for these differences. Simmons et al. showed that depression-related increases in appetite are associated with overactivity of the GOGETTER, or mesolimbic reward circuit.
Consistent with the concept of bidirection, Sharma et al. found in mice that chronic consumption of high-fat food and associated weight gain induced plasticity-related changes in the reward circuit (GOGETTER) that are associated with depression.
Not to leave out the Sleepy Executive, Cserjési et al. studied the relationship between depression and executive function. They found a mediating role of depression between executive self-regulation skills and obesity. This suggests that depression may play a role in making the Sleepy Executive sleepier in those with both depression and weight gain.
Various categories of studies have demonstrated an association between ADHD and symptoms of overweight and obesity.
Consistent with our theme, Seymour et al. found that there appears to be significant overlap in the neurological circuits that mediate ADHD and obesity. Specifically, they found overlap within the motivational system (GOGETTER) and the circuits that mediate response inhibition and regulation (the Sleepy Executive).
PHYSICAL ACTIVITY AND SEDENTARINESS
The relationship between physical activity and weight regulation is not straightforward. For more, see the Diet, Exercise and Calorie Deficit module.
Shan et al. showed that moderate to vigorous physical activity is associated with decreased brain response to high-calorie food cues in the region of the motivational system or GOGETTER, suggesting that physical activity can decrease WANTING. They also showed that sedentary behaviour was correlated with greater reactivity and stronger GOGETTER-generated WANTING.
Again, not to leave out the Sleepy Executive, numerous meta-analyses, including that of Moreau et al., have found that moderate- and high-intensity exercise has a positive impact on executive function, and restraint is a key executive function.
From an evolutionary perspective, the GOGETTER has two roles: 1) produces the drive to GO AND GET food when food may be scarce, and 2) promotes overeating when food is available in order to establish energy stores for an uncertain future.
When we go too long without food, this motivation system gets temporarily strengthened. WANTING gets stronger. A major supporter of this temporary strengthening is the food intake-promoting hormone ghrelin. Ghrelin is produced in the stomach and is at its highest levels before we eat.
Perello and Dickson describe how ghrelin directly signals both the GATEKEEPER (the hypothalamus) and the GOGETTER (the motivation/reward system) to promote GOING AND GETTING, and then eating.
The most likely causes of increased release of ghrelin include:
-
Going too long without food
-
Anticipation of food
-
Weight loss
-
Psychological stress
In the case of going too long without food, the signals that result in ghrelin release include low blood glucose and the release of a hormone called norepinephrine. Simply anticipating tasty, hyper-palatable food may also result in ghrelin release.
Again, working towards your BEST WEIGHT is tough enough. Modulators can make it more difficult. Please advocate for yourself. It is recommended that your health care practitioner(s) actively assess you for the effects of this finite list of modulators and diagnose and treat them if necessary. If modulators are determined to be affecting your weight, please consider treatments such as stress reduction/management strategies, sleep testing for sleep apnea, treatment for insomnia, treatment for depression and ADHD, strategies to increase physical activity, and consideration of avoiding going too long without food.






Leave a Reply